COVID-19 Timeline in Tennessee, from the Governor's Office
From the first confirmed case of COVID-19, Gov. Lee and the State of Tennessee streamlined their response to protect the health and safety of all citizens, provide relief for struggling families and businesses, and ensure our economy rebounds from the unprecedented effects of COVID-19. We’re proud of what’s been accomplished and look forward to a safe and strategic recovery.
For up-to-date information on the State of Tennessee's COVID-19 response, visit tn.gov/covid19 and for additional updates from Tennessee's Economic Recovery Group, visit TNPledge.com.
January 16, 2020
- State Health Operations Center activated due to COVID-19, allowing for the Tennessee Department of Health to maximize capacity and available resources of the state’s metro and regional health departments.
January 21, 2020
- The Tennessee Department of Health developed triage and surveillance processes and guidance.
- Department began a healthcare provider call line to answer clinical questions and screen for laboratory testing at CDC.
January 23, 2020
- The Tennessee Department of Health distributed the first Tennessee Health Alert Network message on COVID-19 to all licensed healthcare providers in Tennessee.
January 24, 2020
- The Tennessee Department of Health developed and published the TDH Novel Coronavirus webpage.
January 31, 2020
- The U.S. Department of Health and Human Services declared a public health emergency for the United States.
February 7, 2020
- Returning traveler monitoring implemented in Tennessee.
February 21, 2020
- Tennessee State Public Health Laboratory validated the PCR test at the Nashville laboratory, becoming one of only five states in the nation to complete the verification of the CDC EUA COVID-19 test.
February 24, 2020
- The Tennessee Department of Health conducted the first COVID-19 test in the state using the CDC EUA test.
March 3, 2020
- The state's deadliest tornado in seven years hits communities in West and Middle Tennessee, killing 25 Tennesseans, injuring more than 300 and causing $1.1 billion in total damages.
March 4, 2020
- Gov. Lee announced the formation of the Coronavirus Task Force to enhance Tennessee’s coordinated efforts to prevent, identify, and treat potential cases of COVID-19.
March 5, 2020
- The Tennessee Department of Health announces the first confirmed case of COVID-19 in Tennessee.
- TDH establishes a public information line, staffed by Tennessee Poison Center.
March 6, 2020
- President Trump and Gov. Lee toured tornado damage in Putnam County.
March 12, 2020
- Gov. Lee issued Executive Order No. 14 declaring a State of Emergency to free up funds for the treatment and containment of COVID-19
March 13, 2020
- Gov. Lee issued further guidance regarding mass gatherings, schools, state employees and the State Capitol Building as more confirmed cases of COVID-19 were identified in Tennessee:
- Congregations and groups are urged to consider alternatives to traditional services by utilizing live streams, pre-recorded messages, and other electronic means.
- Events larger than 250 people are discouraged to limit exposure to COVID-19.
- School districts have been advised to exercise discretion when canceling school for K-12 students. The state will provide further support for districts pursuing this action but urge districts to consider the prevalence of confirmed cases of COVID-19 in their area. In partnership with districts, students who depend on school-provided meals will still receive this support, regardless of school closure.
- State employees who have been trained and certified to work from home within the state’s Alternative Workplace Solutions program will work from home through March 31, 2020.
- State employees have been instructed to cease all non-essential business travel through March 31, 2020.
- The Tennessee State Capitol is closed to tours and visitors through March 31, 2020. Members of the media will continue to have access to the State Capitol building.
- The Tennessee National Guard begins implementation of a comprehensive plan that balances the health protection of Soldiers and Airmen with mission readiness in the event they are called upon in support of Governor Lee’s state emergency declaration. Upgrades to Health Protection Control – Level C (HPCON-C).
March 14, 2020
- The Tennessee Department of Health establishes a second public information line at TEMA.
March 16, 2020
- Gov. Lee announced limiting all remaining legislative business to fulfilling the constitutional requirement of passing a balanced budget, and any associated actions that will ensure Tennessee can keep its doors open.
March 17, 2020
- Gov. Lee urged all school districts in Tennessee to close by March 20 and remain closed through March 31. Gov. Lee announced that during this time the School Food Authorities will have the flexibility to continue to provide meals to at-risk students who rely on meals.
- Gov. Lee also announced the following actions to mitigate the spread of COVID-19 in Tennessee:
- Gov. Lee encouraged childcare facilities to remain open to support community needs and directed The Tennessee Department of Human Services to relax the regulatory burden on child care centers.
- The state will provide $10 million in response and recovery grants to support existing childcare facilities.
- The Tennessee Department of Human Services issued a policy offering emergency cash assistance utilizing TANF funds. Assistance will be up to $1,000 for families of five or more who qualify and who have experienced the loss of a job as a result of COVID-19.
- The Tennessee Department of Labor and Workforce Development is working to determine how to utilize the Unemployment Insurance Trust Fund. The Tennessee Department will extend unemployment benefits to those quarantined by a physician for COVID-19.
- Gov. Lee’s amended budget includes $200 million to provide specific relief to county and city governments.
March 20, 2020
- The Tennessee Department of Health established COVID-19 assessment at rural local health departments.
- The State of Tennessee received the Strategic National Stockpile allocation.
March 22, 2020
- Gov. Lee issued Executive Order No. 17 calling on businesses to utilize “alternative business models” and prohibiting gatherings of 10 or more people. The order also:
- Orders restaurants and bars to offer only drive-thru, take-out, or delivery, and permits closed-container alcohol take-out or delivery;
- Temporarily closes gyms and fitness centers; and
- Limits visitation to nursing homes, retirement homes, and long-term care facilities.
March 23, 2020
- Gov. Lee established a COVID-19 Unified-Command Group to streamline coordination across the Tennessee Emergency Management Agency, Tennessee Department of Health, and Tennessee Department of Military. The Command will be led by Commissioner Stuart McWhorter.
- The Tennessee National Guard established collection points at armories in 74 counties across the state to receive donated PPE and medical equipment for the state’s front line health care workers.
March 24, 2020
- Gov. Lee mobilized 250 members of the Tennessee National Guard, including 150 medical personnel, to assist TDH personnel with expanded testing across the state at 35 remote assessment sites in some of the most rural counties.
- Gov. Lee extended work from home orders for state employees under the Alternative Workplace Solutions program, until April 24.
- Gov. Lee extended statewide school closures until April 24.
- Gov. Lee announced a series of administrative actions to mitigate the impact of COVID-19, including:
- Delaying the deadline to file franchise and excise taxes until July 15;
- Suspending the issuance of REAL ID through May 18;
- Waiving emissions testing requirements through May 18;
- Filing an emergency petition, in partnership with the Attorney General, an emergency petition asking the Tennessee Public Utility Commission to prohibit utilities from disconnecting services for non-payment during the state of emergency; and
- Directing The Tennessee Department of Commerce and Insurance to issue guidance to providers requesting flexibility for employers and individuals.
March 25, 2020
- Gov. Lee announced the purchase of additional testing supplies using CDC funding.
- The Tennessee Department of Human Services announced the use of emergency response and recovery grants for existing child care facilities, allowing churches, gyms, or non-profits to register with The Tennessee Department to open an emergency temporary child care facility.
March 26, 2020
- Gov. Lee announced the creation of Tennessee Talent Exchange, a public-private partnership with the Tennessee Grocers and Convenience Store Association, Tennessee Retail Association, and Hospitality TN to match out of work Tennesseans with companies currently experiencing business surges.
- Gov. Lee issued Executive Order No. 20 to better mobilize health care workers, by:
- Loosening restrictions around retired medical professionals returning to the workforce;
- Temporarily suspending continuing education requirements so professionals can continue to work through the pandemic;
- Calling for the availability of phone assessments for individuals with mental illness or emotional disturbances; and
- Expanding telemedicine efforts.
- Gov. Lee extended emergency cash assistance (TANF) for up to two months to families significantly impacted by COVID-19. Families who have lost employment or at least 50% of their earned income as a result of the pandemic are eligible.
- Gov. Lee announced the creation of the Talent Exchange, a public-private partnership with the Tennessee Grocers and Convenience Store Association, Tennessee Retail Association, and Hospitality TN to match out-of-work individuals with companies currently experiencing business surges.
- LaunchTN led an evaluation of technology-based solutions for data analysis on disease spread, contact tracing, collective impact, and community planning for disaster response.
- The State of Tennessee Launched the “Do Your Part, Stay Apart” Public Service Campaign.
March 27, 2020
- TEMA coordinates to receive 25,000 sq. feet of donated warehouse space from Genesco Corp. to serve as a PPE and supply distribution point manned by TEMA and Tenn. Guard personnel.
March 29, 2020
- The COVID-19 Unified-Command Group announced coordination with the Gallatin Center for Rehabilitation and Healing to address the COVID-19 outbreak at the facility.
- The transport of 23 residents to Sumner Regional Medical Center via an ambulance strike team of EMS Professionals on Friday, March 27;
- Engagement of the National Guard on-site to assist with testing;
- Isolation of staff members who tested positive; and
- Deep cleaning and disinfecting of the facility.
March 30, 2020
- Gov. Lee issued Executive Order No.22 issuing “Safer at Home” guidelines, which will remain in effect until April 14.
- The Unified-Command Group announced the Tennessee Innovation Crowdsource Platform, a partnership with LaunchTN to sync together businesses, entrepreneurs, and startups to solve the challenges facing our state during this unprecedented time.
- LaunchTN began discussions with Renfro, Corp, a global sock brand company, headquartered in Mount Airy, N.C., with a manufacturing and distribution operation in Cleveland, Tenn., to make cloth face masks available to as many Tennesseans as possible.
March 31, 2020
- The Tennessee Department of Mental Health and Substance Abuse Services began working with behavioral health providers to expand service to individuals who need professional behavioral health help, including expanded telehealth services and mobile behavioral health care units.
- The Centers for Medicare & Medicaid Services (CMS) approved Tennessee’s request for a Section 1135 Medicaid waiver. The approved waiver enables Tennessee to provide flexibilities in Medicaid provider screening and enrollment, forgo certain pre-admission screening and annual resident review assessments, and allow for reimbursement facility services in alternative settings.
April 1, 2020
- Gov. Lee announced coordination with the Army Corps of Engineers to prepare for a surge of hospitalizations.
April 2, 2020
- Gov. Lee issued Executive Order No. 23 requiring Tennesseans to stay at home except for essential activities.
- President Trump approved Tennessee’s major disaster declaration, accelerating coordination with the Army Corps of Engineers, and expanding statewide capacity by 7,000 beds.
- The Tennessee Department of Health began registering volunteers for COVID-19 medical and non-medical responders using the Medical Reserve Corps
April 3, 2020
- Gov. Lee issued Executive Order No. 24, which:
- Grants with Commissioner of Health authority to expand telemedicine and allow post-degree, pre-licensed mental or behavioral health professionals to treat patients;
- Suspends and extends deadlines for filing and paying taxes and applying for tax relief;
- Grants the Commissioner of Labor and Workforce Development discretion to require expedited information in processing unemployment benefits claims;
- Extends the law against price gouging for an additional 15 days;
- Suspends the expiration of marriage licenses;
- Extends the deadline for law enforcement officers to complete certain introductory POST Commission courses;
- Extends the due date for driver license reinstatement installment payments;
- Provides flexibility for Tennessee Corrections Institute county jail plans; and
- Suspends requirements regarding the deposit of funds at the walk-in state service location.
- With shortages of personal protective equipment, the Tennessee Department of Health creates Memorandum of Understanding with first responders to temporarily provide COVID-19 positive case information.
April 6, 2020
- Gov. Lee announced $200 million in grants to be distributed to every county and city government across the state for one-time, local expenses.
- Gov. Lee announced $10 million in Small and Rural Hospital Readiness Grants to support hospitals.
- The Tennessee Division of TennCare submitted a waiver to the federal government seeking matching dollars to address the uninsured population.
April 7, 2020
- Gov. Lee announced support for the Paycheck Protection Program, which offers fully forgivable loans to help small businesses maintain payrolls.
April 8, 2020
- Gov. Lee issued Executive Order No. 25, extending the postponement of elective medical and dental procedures until April 30.
- Gov. Lee announced a partnership with HealthStream, a Nashville-based company that will provide quick and free training to retired or furloughed medical workers willing to rejoin the workforce to fight COVID-19.
April 9, 2020
- Gov. Lee announced a partnership with Nextdoor to provide official, real-time information to Tennesseans about the state’s response.
April 13, 2020
- At least nine dead, dozens hospitalized and 150 buildings damaged after storms and tornado rip through Hamilton and Bradley Counties.
- Gov. Lee traveled to Chattanooga, TN to survey storm damage and visit with communities that were impacted by deadly storms.
- Gov. Lee issued Executive Order No. 27 extending the state’s Stay at Home Order until April 30.
- Gov. Lee announced the development of the Economic Recovery Group to coordinate legislative leadership, local leadership, health care professionals, and industry representatives to reboot the economy.
April 15, 2020
- Gov. Lee announced expanded COVID-19 testing in coordination with the National Guard, free to all Tennesseans, regardless of symptoms,
- Gov. Lee called on schools to remain closed for the remainder of the academic year.
- Gov. Lee Appointed Butch Eley as Commissioner of the Tennessee Department of Finance and Administration
April 16, 2020
- Gov. Lee appointed the Tennessee Department of Tourist Development Commissioner Mark Ezell to lead the Economic Recovery Group.
- Gov. Lee announced the creation of the Stimulus Financial Accountability Group to oversee the prudent fiscal management of CARES Act funding received by the state.
April 17, 2020
- Gov. Lee issued Executive Order No. 28, removing regulatory barriers to facilitate the treatment of COVID-19, including:
- Extending the deadline for firefighters to obtain a medical examination;
- Suspending the collaborating physician requirement for nurse practitioners and physician assistants;
- Allowing nursing school graduates to work during the emergency order under the supervision of a licensed nurse;
- Allowing nurse practitioners and physician assistants to write orders for home health services;
- Expanding the facilities in which autopsies may be performed;
- Allowing medical laboratory personnel to work from home in reviewing data and reporting results;
- Protecting HIPAA information sent by the DoH to first responders and law enforcement personnel; and
- Extending the price gouging law for an additional 15 days.
- The Tennessee Department of Human Services announced new child care assistance to support families serving in essential workforce positions.
- Gov. Lee announced expanded testing, with the Tennessee National Guard establishing 15 drive-through testing sites.
April 20, 2020
- Gov. Lee announced that Tennessee’s Stay at Home order will expire on April 30th, and a vast majority of businesses in 89 of 95 counties will be allowed to reopen on May 1st.
- Unified-Command Group tests more than 11,000 Tennesseans
April 21, 2020
- Gov. Lee announced that the first four grants of a $10 million grant program were distributed to support hospitals facing financial strain.
- The Tennessee Department of Health’s Office of Minority Health Disparities Elimination provided an overview of efforts to engage minority communities seeking testing and treatment. Actions include:
- Engagement of non-profits, faith leaders, legislators, and local leaders;
- Expanded testing efforts to coordinate with local health clinics and safety-net clinics;
- Focused resources to improve race and ethnicity data collection; and
- Additional public service announcements focused on minority health concerns
- LaunchTN convened an entrepreneur center alongside other Tennessee CEOs to formulate strategies to get entrepreneurs, innovators, and startups back to work.
April 22, 2020
- The Tennessee COVID-19 Unified-Command Group released data regarding the state’s long-term care facilities and outlined a plan for preventing future cases and mitigating present clusters of cases within these facilities.
April 23, 2020
- Gov. Lee announced the following initial guidance on retail industry reopening:
- Restaurants operating at 50% capacity and following Tennessee Pledge guidance will be allowed to open on Monday, April 27; and
- Retail outfits operating at 50% and following Tennessee Pledge guidance will be allowed to open on Wednesday, April 29.
- The Tennessee Department of Labor and Workforce Development issued an update on actions to support Tennesseans including system upgrades and benefit distribution.
- The Tennessee Department of Environment and Conservation Commissioner David Salyers announced that most state parks will reopen for day-use only on Friday, April 24.
- LaunchTN worked with the University of Memphis and Tennessee Department of Mental Health and Substance Abuse Services Commissioner Marie Williams to introduce a suicide prevention technology strategy for the state during the COVID-19 pandemic.
- Trisha Yearwood, Garth Brooks joined Tennessee’s “Do Your Part, Stay Apart” Public Service Campaign.
April 24, 2020
- Tennessee’s Economic Recovery Group issued guidance to restaurants and retailers as part of “Tennessee Pledge,” the state’s rollout approach to safely reopening businesses in 89 of 95 counties.
- Gov. Lee issued Executive Order No. 29, amending Executive Order No. 17 and allowing restaurants to begin reopening on April 27.
- The Tennessee Department of Health established an Enhanced Testing Strategy team to coordinate laboratory testing for vulnerable populations including prisoners, staff and residents at nursing homes, and minority populations.
April 27, 2020
- Tennessee’s Economic Recovery Group released Universal Guidance for Tennessee Businesses, found here.
- Tennessee’s Economic Recovery Group issued safe reopening guidance for restaurant and retail industries.
- The Unified-Command Group announced the free testing of more than 7,000 Tennesseans – regardless of symptoms – at drive-through sites across the state.
- Gov. Lee directed the Tennessee Department of Finance & Administration to temporarily freeze any new non-mission critical hires to the state’s workforce.
- Gov. Lee announced that elective medical procedures will be allowed to resume on May 1.
April 28, 2020
- Tennessee’s Economic Recovery Group issued guidance for gyms and exercise facilities to safely reopen beginning May 1.
- Gov. Lee issued Executive Order No. 30, repealing Executive Order Nos 17, 21, 22, 23, 27, and 29. The Order will, among other things:
- Maintain the prohibition on gatherings of 10 or more people, with the exception of places of worship, weddings, and funerals;
- Allow certain businesses to return to work in compliance with health guidelines;
- Mandate that entertainment and recreational gathering venues remain closed;
- Provide guidance regarding limited service in restaurants and take-out and delivery of alcohol;
- Provide guidance to nursing homes and like long-term care facilities regarding visitation; and
- Outline requirements to the public writ large.
April 29, 2020
- Gov. Lee issued Executive Order No. 31, extending the prohibition of non-emergent dental services until May 6.
- Gov. Lee announced that close contact services, such as salons and barbershops, will be able to safely reopen beginning May 6.
April 30, 2020
- The Tennessee Economic Recovery Group issued guidance for close contact services to safely reopen beginning May 6.
- Gov. Lee joined President Trump for a White House Briefing on protecting America’s seniors during the COVID-19 pandemic.
- Gov. Lee announced that his Administration has been working with the Tennessee Medical Association to prepare for the expiration of Executive Order No. 25, and the resumption of elective and non-urgent medical procedures beginning May 1.
May 1, 2020
- The Unified-Command Group announced a mass testing strategy for all Tennessee Department of Correction staff and inmates.
- Gov. Lee’s Office of Faith-Based and Community Initiatives issued guidance for faith communities on safely gathering together in houses of worship.
- Gov. Lee issued Executive Order No. 32, outlining plans to further mitigate COVID-19, including:
- Waiving fees to obtain copies of business entity filings for purposes of seeking relief under a state of a federal program;
- Extending the price gouging law for another 15-day period;
- Allowing reimbursement for physical, occupational, and speech therapy via telemedicine for workers’ compensation recipients;
- Allowing for discretion in the utilization of National Guard members in connection with TDOC operations or security;
- Granting flexibility to the Commissioners of Intellectual and Developmental Disabilities with respect to hiring requirements made difficult by COVID-19;
- Allowing corporations to conduct remote shareholder meetings; and
- Extending the deadline for qualified TNInvestco to file annual audited financial statements with the Department of Economic and Community Development.
May 4, 2020
- Gov. Lee announced that more than 23,000 Tennesseans received free COVID-19 tests at more than 67 drive-through testing sites as part of the Unified-Command Group’s efforts to broaden testing access.
May 5, 2020
- The Unified-Command Group announced two strategic partnerships to provide Tennessee households and health care workers with protective face coverings and PPE.
- Gov. Lee issued Executive Order No. 33, allowing the safe reopening of close contact services.
- Gov. Lee announced that, under guidelines set by the Tennessee Board of Dentistry and the American Dental Association, dental procedures will resume on May 6.
- LaunchTN worked with the Economic Recovery Group to establish the Tennessee PPE Vendor Directory.
May 6, 2020
- The Tennessee Economic Recovery Group released additional guidance for recreation, offices, lodging, construction and manufacturing, small group, and non-contact recreation businesses to reopen on May 8.
May 7, 2020
- Gov. Lee issued Executive Order No. 34, allowing government bodies to hold meetings remotely until June 30.
- Gov. Lee issued Executive Order No. 35, allowing the reopening of small group, non-contact entertainment, and recreational venues.
May 8, 2020
- Gov. Lee announced next steps for Tennessee’s Unified-Command Group.
May 12, 2020
- Gov. Lee issued Executive Order Nos 36 and 37, extending the state of emergency from May 18 until June 30.
- The Tennessee Department of Intellectual and Developmental Disabilities and the Tennessee Department of Health announced a collaboration to increase testing accessibility for intermediate care facilities and members of the Employment and Community First CHOICES program.
- Gov. Lee issued Executive Order No.s 36 and 37, extending the state of emergency from May 18 until June 30.
May 13, 2020
- Gov. Lee announced coordination between the Unified-Command Group and the Metropolitan Development and Housing Agency (MDHA) to provide free, voluntary COVID-19 testing, by Tenn. National Guard medics, for families and residents at 14 MDHA communities in Nashville.
May 14, 2020
- Memphis 401-bed Alternative Care Site (ACS) at Commercial Appeal building completed.
May 15, 2020
- Gov. Lee announced coordination between the Unified-Command Group, the Knoxville Community Development Corporation, the Knox County Health Department, and the Memphis Housing Authority to provide free, voluntary COVID-19 testing, by Tenn. National Guard medics, for families and residents at six KCDC properties in Knoxville and 5 MHA properties in Memphis.
- The Economic Recovery Group announced the lifting of capacity restrictions on restaurants and retail effective May 22.
- The Group also issued guidance to facilitate the reopening of large, non-contact attractions on or after May 22.
May 18, 2020
- The Governor announced the completion of the Memphis Alternative Care Site that can treat over 400 additional individuals.
May 19, 2020
- Gov. Lee announced the final distribution of Small and Rural Hospital Readiness Grants to support smaller hospitals that are facing financial strain due to the ongoing COVID-19 response.
May 20, 2020
- Gov. Lee announced coordination between the Unified-Command Group and the Chattanooga Housing Authority to provide free, voluntary COVID-19 testing, by Tenn. National Guard medics, for families and residents at four CHA communities in Chattanooga.
- The Economic Recovery Group issued updated guidance for restaurants and retail, along with new guidelines that enable attractions and larger venues to reopen with social distancing and capacity restrictions on or after May 22.
May 22, 2020
- Gov. Lee issued Executive Order No. 38, allowing groups of up to 50 people to participate in social and recreational activities while encouraging strong social distancing measures.
May 27, 2020
- Gov. Lee calls the State Funding Board to review economic projections and assess the impacts of COVID-19 on state revenues and the budget.
- Healthcare Facilities Board unanimously approved new rules from the Department of Health requiring testing of all long-term care facilities. Once a nursing home has completed initial testing, each facility shall test all staff members for COVID-19 at least once every seven days beginning the later of June 30 or the date the facility completes initial testing.
- Tennessee reached the milestone of testing 6% of the state’s population with 400,000+ tests conducted since March. First responders set to receive shipments of personal protective equipment to guard against COVID-19 transmission in the line of duty.
May 28, 2020
- The Tennessee Economic Recovery Group issues guidance for non-contact sports, overnight camps, and Tennessee’s higher education institutions.
- Metro Nashville General Hospital announced as Middle Tennessee alternate care site, providing 67 additional beds for low-acuity COVID-19 patients.
County Unemployment Rates Reach Historic Highs in Tennessee
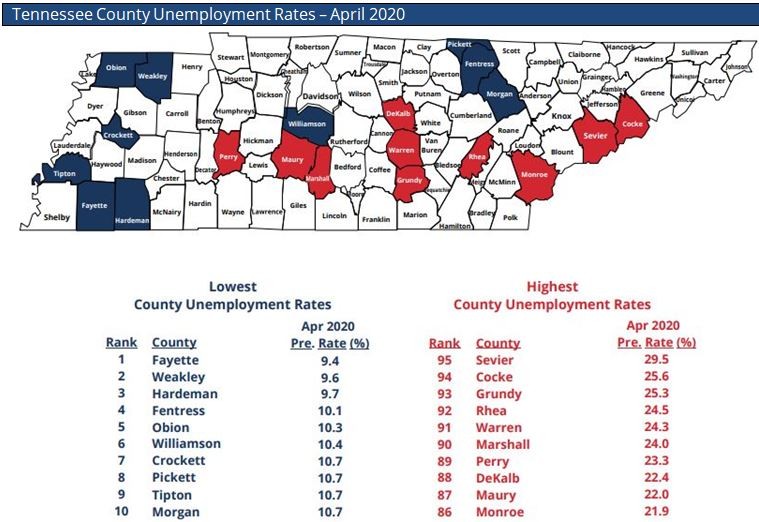
NASHVILLE – Statistics released today by the Tennessee Department of Labor and Workforce Development show a staggering increase in unemployment for each of Tennessee’s 95 counties in April as many businesses closed to help slow the spread of COVID-19.
The unprecedented and historic spike in unemployment impacted some counties more drastically than others, but no area of Tennessee escaped the pandemic’s effect on the state’s workforce.
Fayette County had Tennessee’s lowest unemployment rate in April. At 9.4%, the county’s rate increased by 6.1 percentage points when compared to its revised March rate of 3.3%
Weakley County had the second-lowest unemployment rate for the month at 9.6%, followed by Hardeman County at 9.7%.
Fayette, Weakley, and Hardeman were the only counties in the state with unemployment rates below 10% in April.
Sevier County recorded Tennessee’s highest unemployment rate for the month. The county’s new jobless figure of 29.5% represents a staggering spike of 26 percentage points when compared to its revised March rate of 3.5%.
Neighboring Cocke County had the second-highest jobless rate in April at 25.6%, a 20.9 percentage point increase from the previous month. Grundy County ranked third-highest with a rate of 25.3%, which is a 21.1 percentage point spike when compared to March’s rate.
When comparing Tennessee’s three largest cities, Nashville had the highest unemployment rate in April. The city’s rate of 15.9% is a 13.5 percentage point increase over its revised March rate of 2.4%. Memphis recorded a rate of 14.3%, a spike of 10.1 percentage points from the previous month, and Knoxville’s April rate of 14.7% is an 11.8 percentage point jump.
Statewide, unemployment reached a historic high in April. The seasonally adjusted rate of 14.7% surpassed the previous all-time high figure of 12.9% in January 1983.
Unlike the statewide unemployment rate, county unemployment statistics are not seasonally adjusted.
A complete in-depth analysis of unemployment data for each of Tennessee’s counties is available here.
The state of Tennessee will release statewide unemployment rate for May 2020 on Thursday, June 18, 2020, at 1:30 p.m. CT.
Free Summer Meals for Plateau Children Begin June 8
The University of the South in partnership with the South Cumberland Community Fund and 12 local community partners are pleased to announce their sponsorship of the 2020 Summer Food Service Program (SFSP). The SFSP is administered in Tennessee by the Department of Human Services under an agreement with the U.S. Department of Agriculture (USDA).
The program known as the South Cumberland Summer Meal Program will begin distributing meals June 8, at 12 sites located in Grundy, Franklin, and Marion counties. The 2020 Summer Food Service Program will distribute meals through July 30.
Meals will be provided to all children 18 years and younger at no charge regardless of race, color, national origin, sex, age or disability. Meals will be provided at the locations, dates and times as follows:
Tracy Elementary School, 276 3rd St., Tracy City, June 10–July 27, Wednesday, June 10, 10 a.m.–noon, Monday, June 15–July 27, 10 a.m.–noon
DuBose Healthy Roots, 635 College St., Monteagle, July 6–10, Monday and Friday, 10 a.m.–noon
Coalmont Elementary School, 7862 SR 56, Coalmont, June 10,–July 27, Wednesday, June 10, 10 a.m.–noon, Monday, June 15–July 27, 10 a.m.–noon
Pelham Elementary School, 2402 SR 50, Pelham, June 10–July 27, Wednesday, June 10, 10 a.m.–noon, Monday, June 15–July 27, 10 a.m.–noon
Palmer Elementary School, 226 Palmer Rd., Palmer, June 11–July 28, Thursday, June 11, 10 a.m.–noon, Tuesday, June 16–July 28, 10 a.m.–noon
North Elementary School, 309 Main St., Altamont, June 11–July 28, 202, Thursday, June 11, 10 a.m.–noon, Tuesday, June 16–July 28, 10 a.m.–noon
Swiss Memorial School, 477 55th Ave., Gruetli Laager, June 11–July 28, Thursday, June 11, 10 a.m.–noon, Tuesday, June 16–July 28, 10 a.m.–noon
Monteagle Elementary School, 120 E Main St., Monteagle, June 10–July 27, Wednesday, June 10, 10 a.m.–noon, Monday, June 15–June 29, 10 a.m.–noon, July 13–July 27, 10 a.m.–noon
Rain Teen Center, 626 Bennett Cemetery Rd., Decherd, June 10–July 29, 2020, Wednesday, 5–7:30 p.m.
Grace Center for Hope, 912 S College St., Winchester, June 9–July 30, Tuesday, Wednesday, Thursday, 11:30 a.m.–1:30 p.m.,
Franklin Co. Prevention Coalition, 900 S Shepard St., Winchester, June 8–July 28, Monday and Tuesday, 5:30–7:30 p.m.
Camp Rain, 626 Bennett Cemetery Rd., Decherd, June 15–July 11, 2020, June 15–18 and July 5–11, 8–10 a.m., and 11:30 a.m.–1:30 p.m.
If you wish to file a Civil Rights program complaint of discrimination, complete the USDA Program Discrimination Complaint Form, found online at
Send your completed complaint form or letter to us by mail to:
U.S. Department of Agriculture, Director
Office of Adjudication, 1400 Independence Avenue, S.W. , Washington, DC 20250-9410
By fax at (202) 690-7442
or email at <program.intake@usda.gov>.
Individuals who are deaf, hard of hearing or have speech disabilities may contact USDA through the Federal Relay Service at (800) 877-8339; or (800) 845-6136 (Spanish).
USDA is an equal opportunity provider and employer.
Follow the Summer Meal Program on Facebook https://www.facebook.com/SouthCumberlandSMP/
Quick Links from the TN Department of Health
Mental Health

- TN Statewide Crisis Line: 855-CRISIS-1 (855-274-7471). 24/7/365 call system to help anyone experiencing a mental health crisis
- Crisis Text Line: text TN to 741-741 to connect to a trained counselor
- Substance Abuse and Mental Health Services Administration (SAMHSA) Disaster Distress Helpline Toll-Free: 1-800-985-5990 (English and español) SMS: Text TalkWithUs to 66746
- Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS)
- Tennessee Suicide Prevention Network (TSPN)
- Protecting Your Mental Health
From the TN Department of Health, May 27, 2020
Coronavirus Disease (COVID-19)
COVID-19 Public Information Number 877-857-2945 or 833-556-2476 Available 10 a.m. – 8 p.m. Monday – Friday and 10 a.m.- 4 p.m., Saturday and Sunday.
From the TN Dept. of Health, May 22, 2020
Coronavirus Disease (COVID-19)
COVID-19 Public Information Number 877-857-2945 or 833-556-2476 Available 10 a.m. – 8 p.m. Monday – Friday and 10 a.m.- 4 p.m., Saturday and Sunday.
COVID-19 Bulletin #34 - May 22, 2020
Today, Governor Bill Lee provided an update on Tennessee’s efforts regarding COVID-19. Gov. Lee’s conferences can be viewed here. Visit tn.gov/covid19 for up-to-date administrative action.
Key Updates
Testing Strategy Continues to Meet Goals
Tennessee continues to be a national leader in COVID-19 testing. Tennessee has already tested 2.5% of the state’s population and is on track to reach 3% by the end of May, surpassing the White House’s testing criteria of 2% per month for a safe reopening.
From May 1 – May 20, Tennessee conducted roughly 177,000 COVID-19 tests, more than all previous weeks combined. The state currently conducts, on average, upwards of 8,700 tests per day and was listed by the Harvard Global Health Institute as one of 7 states to reach a benchmark for COVID-19 testing.
Additionally, Unified Command has facilitated testing of the state’s inmate population, major metro urban housing development communities, intellectual and developmental disability communities, long-term care facilities, and veterans homes, with continued availability for those in the community regardless of symptoms.
For a full primer on Unified Command’s testing efforts, click here.
Executive Order No. 38
Today, Gov. Lee issued Executive Order No. 38, which allows groups of up to 50 people to participate in social and recreational activities while encouraging strong social distancing measures. The order’s provisions include:
- Effective Friday, May 22, this order supersedes and repeals Executive Order Nos. 30, 33, and 35.
- The order permits more Tennesseans and businesses to return to work in all industries where that can be safely accomplished by following health guidelines and maintaining social distancing from persons outside of your household, while continuing to urge employers to allow or require remote work/telework if possible.
- Requirements with respect to social and recreational gatherings, such as festivals, fairs, parades, large parties or picnics, noncontact sporting events and activities, summer camps, and other types of social or recreational gatherings, are clarified to focus on the importance of social distancing from persons outside your household and avoiding social/recreational groups of 50 or more persons, consistent with recent conversations and input from counties across the state, including the six locally run county health departments with independent orders or plans in place.
- This limitation does not cover places of worship, for which there are guidelines for safe operation of worship services and gatherings if in-person services are conducted, but the order strongly encourages places of worship to continue virtual or online services where possible.
- This limitation does not apply to weddings, funerals, and related events, but encourages postponement of large-gathering components of such events.
- Non-contact sporting events and activities and summer camps should be conducted in accordance with operational guidance from the Governor’s Economic Recovery Group (e.g., Tennessee Pledge), which is forthcoming soon.
- Contact sporting events and activities, where there is a requirement or substantial likelihood of routine close contact and adequate social distancing is not feasible, are prohibited, but this does not apply to collegiate or professional sports conducted under the rules or guidelines of their respective governing bodies. This also does not prohibit training or otherwise practicing the elements of such sports that do not involve close contact with persons.
- Nursing homes and similar retirement and long-term-care facilities must remain closed to visitors, unless in the discretion of the facility the visit involves critical assistance for the resident or is to a resident receiving end-of-life care, provided that such a visit may be accomplished without unreasonable risk. These facilities must also ensure that residents with disabilities are afforded necessary visitation by service providers and other persons.
- Administrators of nursing homes and similar retirement and long-term-care facilities are strongly encouraged to provide COVID-19 testing to all residents and staff or take substantial steps toward completing such testing by May 31, 2020. Financial and operational support for such testing is available from the Tennessee Department of Health and Tennessee National Guard.
- Senior centers or equivalent facilities remain closed to members or the public.
- Attractions and larger venues may reopen, but should follow the Economic Recovery Group Guidelines (e.g., Tennessee Pledge), including with respect to social distancing and capacity limits
- Bars may reopen, but may only serve customers seated at appropriately spaced tables and must follow the Economic Recovery Group Guidelines (e.g., Tennessee Pledge) for restaurants.
- Tennesseans are urged to continue limiting activity and staying home as much as possible to preserve and build on the health progress we’ve made.
- All employers and businesses that choose to open are expected to comply with the Governor’s Economic Recovery Group Guidelines for operating safely, as well as general health guidelines from the CDC and other government entities.
- Persons and businesses are urged to take special care to protect and provide for the well-being of vulnerable populations, including by offering delivery or special shopping hours if possible.
- Persons with COVID-19 or COVID-19 symptoms are required to stay at home, and employers may not require or allow employees with COVID-19 to work.
- Persons are urged to wear a cloth face covering in places where in close proximity to others, especially where social distancing is difficult.
- Take-out and delivery alcohol sales by restaurants and limited-service restaurants will continue to be permitted to encourage customers to utilize take-out or delivery options.
- For the 89 counties without a locally run county health department (all but Davidson, Hamilton, Knox, Madison, Shelby, and Sullivan), this order supersedes any contrary orders or measures, meaning that the counties cannot issue independent orders that would limit application of Executive Order No. 38, though counties may continue issuing or enforcing orders or measures on other matters related to COVID-19, such as opening or closure of their governmental buildings, governing their employees, or dealing with the operation of their local government.
- The county health departments in the 6 counties with locally run county health departments (Davidson, Hamilton, Knox, Madison, Shelby, and Sullivan) shall have authority to issue orders or measures that permit or restrict to a different degree than this order the opening, closure, or operation of businesses, organizations, or venues, or the gathering of persons, except for in the case of places of worship. Otherwise, this order governs on the topics it covers.
The full text of the order is available here.
Continued Support for Tennessee Families
On Monday, Gov. Lee visited the YMCA of Memphis & the Mid-South to help volunteers distribute meals. This program distributes 900+ meals per day to families in the Shelby Co. community. Additional information on the program is available here.
The Tennessee Dept. of Human Services established the COVID-19 Essential Employee Childcare Payment Assistance Program to provide support for essential workers serving our communities through this pandemic. The program has been expanded until mid-August to support essential employees through the summer. All categories of essential workers identified in EO 22 are now eligible for the program. The full list is located at TN.gov.
The Department has also partnered with YMCA and the Boys & Girls Clubs of Tennessee to establish free child care for the school aged children of essential workers. Full listing of YMCA and Boys & Girls Club temporary/emergency care locations is available for the YMCA here and the Boys & Girls Clubs here.
Education Update
PBS Teaching Tennessee virtual learning program will continue through the summer, allowing students and families to have access to education and instructional content during time away from the classroom. The full schedule is available here.
All Tennessee families will continue to have access to ReadyRosie, a virtual early childhood education platform made possible through partnership with the Governor’s Early Literacy Foundation, through September. More information on ReadyRosie is available here.
Tennessee State Funding Board
In order to better understand the economic impact that has occurred as a result of COVID-19, as well as the implications of those effects, the Governor will be convening a meeting of the State Funding Board, which include state economists as well as economists from the Atlanta Federal Reserve, on Wednesday, May 27, at 10am in Senate Hearing Room I. With the exception of the Funding Board Members, who will appear in-person, the meeting will be conducted through electronic means announced in detail on the Comptroller’s website.
Current Department of Health Testing Results (as of 2 p.m. 5/22)
Confirmed Cases | Hospitalizations | Fatalities | Recovered | Total Tested |
19,394 | 1,560 | 315 | 12,566 | 368,170 |
For more information on COVID-19 in Tennessee, please visit the Tennessee Department of Health’s website here.
From the TN Dept. of Health
Coronavirus Disease (COVID-19)
COVID-19 Public Information Number 877-857-2945 or 833-556-2476 Available 10 a.m. – 8 p.m. Monday – Friday and 10 a.m.- 4 p.m., Saturday and Sunday.
COVID-19 Has Staggering Impact on Tennessee Unemployment

NASHVILLE – Newly released data from the Tennessee Department of Labor and Workforce Development revealed the state’s highest-ever unemployment rate amid the COVID-19 health emergency.
The preliminary seasonally adjusted statewide unemployment rate for April 2020 is 14.7%, which is an unprecedented spike of 11.4 percentage points when compared to March’s revised rate of 3.3%.
This is Tennessee’s highest unemployment rate in a generation. Before the pandemic, the state’s all-time highest seasonally adjusted rate was 12.9%, which occurred in back to back months in December 1982 and January 1983.
Total nonfarm employment in Tennessee decreased by 376,900 jobs between March and April. The largest decreases occurred in leisure/hospitality, manufacturing, and professional/business services sectors.
Over the last 12 months, nonfarm employment decreased by 341,000 jobs. Like the month-to-month data, the largest decreases for the year occurred in the leisure/ hospitality, manufacturing, and professional/business services sectors.
Since March 15, Tennessee has seen an unprecedented surge in unemployment claims filed. During the week ending May 16, the state paid more than 319,000 claimants nearly $359 million in unemployment benefits.
Nationally, seasonally adjusted unemployment experienced a similar spike as in Tennessee. The April 2020 rate for the United States is 14.7%. That figure represents a 10.3 percentage point increase from the previous month’s rate.
The statewide unemployment rate is seasonally adjusted to eliminate the influences of weather, holidays, the opening and closing of schools, and other recurring seasonal events from an economic time series.
You can find a complete analysis of Tennessee’s April 2020 unemployment data here.
Tennesseans searching from new employment can find more than 150,000 current job openings on the state’s workforce development website, www.Jobs4TN.gov. The site also has information about job retraining opportunities, interviews, and resume techniques, as well as local job data.
The state of Tennessee will release the April 2020 county unemployment rates Thursday, May 28, 2020, at 1:30 p.m. CT.
Czarnecki Reports on the Virus Mitigation Efforts
by Bailey Basham, Messenger Staff Writer
A representative from the Tennessee Department of Health spoke to members and guests of the Monteagle-Sewanee Rotary Club this month about the state’s response to COVID-19.
Glenn Czarnecki, regional director for the Southeast Region of the Tennessee Department of Health, spoke to the group about the department’s efforts to mitigate the spread of the respiratory illness caused by the coronavirus.
Rotary president John Solomon said Czarnecki informed the group of some of the department’s actions thus far, including their work to make testing more widely accessible and to begin reopening the state safely.
“Glenn works specifically with rural communities, and the fact that he is plugged into this area was a comfort,” Solomon said. “Tennessee is among the top states as far as the percentage of the population that has been tested. It was just a good opportunity to talk about something that is on everyone’s mind and to get an update directly from someone at the department.”
Tennessee’s first case of COVID-19 was reported on March 4, 2020. Over the subsequent weeks, case numbers increased rapidly. On April 2, Governor Lee signed his Safer at Home order to implement statewide restrictions on non-essential business and travel in order to “flatten the curve” and quickly slow the spread of disease.
In the weeks since, roughly five percent of the population in Tennessee has been tested for the coronavirus, which can often present asymptomatically.
As of this reporting, state health workers have tested nearly 350,000 Tennessee residents, and of those thousands, there have been just over 18,000 positive cases. The Department of Health reported Tuesday that the total of recovered cases was rapidly approaching 11,000.
“The better we understand it, the quicker we can get back to a sense of normalcy,” said Czarnecki.
Czarnecki added that disease monitoring, increased testing, increased health care capacity and an increase in available personal protective equipment are all responsible for slowing the spread of the virus in Tennessee.
For more information about the state’s response to the virus or on how to protect yourself and your community, call the public information number at (877) 857-2945 or (833) 556-2476 from 10 a.m. to 8 p.m. Monday through Friday and 10 a.m. to 4 p.m. on Saturday and Sunday.
If you think you may have been exposed to the coronavirus, contact your doctor and self-isolate. You should get help immediately if you have trouble breathing, persistent chest pain or pressure, new confusion or bluish lips or face, according to the CDC.
To stay up-to-date, visit the department of health’s COVID-19 landing page at <https://www.tn.gov/health/cedep/ncov.htm
Narrowing of Highway 41A Proposed Costs to SUD
by Leslie Lytle, Messenger Staff Writer
In conjunction with plans to narrow Highway 41A, the Sewanee Utility District will be required to relocate sewer and water supply lines. At the May 19 meeting of the board of commissioners, SUD manager Ben Beavers reviewed the contract from the Tennessee Department of Environment and Conservation (TDOT). TDOT regulations stipulate utilities must bear the cost of relocating service lines for road projects if there is not public money available for relocation. The cost for the sewer portion alone is $400,000 in the worst-case scenario.
Board President Charlie Smith observed the developer typically paid for relocating utilities in development projects.
“The way the law is written, we will have to pay,” said Beavers. “How we recover the money is up to us. There’s nothing to say we can’t pass a special development fee for the State Route 15 corridor.” Note: State Route 15 is the state route name for Highway 41A.
The total cost for relocating sewer and water lines is half a million dollars if the plans are not changed. Beavers said there would be a utilities stakeholders meeting with TDOT next week. TDOT regulations stipulate service lines must cross the right-of-way at a 90-degree angle. All but one of SUD’s service lines are very close to the 90-degree benchmark and some are in compliance. Beavers hopes for some relaxing of the standard.
“All the sewer lines were redone in the past 15-20 years,” Beavers said. “There’s nothing wrong with them.”
“The prudent thing is to wait until we get all the facts,” Beavers said. “Once we get a final price, we need to get an official response from the University.” The highway is being narrowed in conjunction with the University’s Sewanee Village project.
The board also discussed SUD’s revenue loss due to the University sending students home and canceling summer programs because of the COVID-19 pandemic. Beavers estimated the loss at $35,000 per month and projected a $200,000 loss for the year, a 28 percent decrease in anticipated revenue. “Once the students return, we’ll be almost back to normal,” Beavers said.
Looking for ways to mediate revenue loss, Beavers suggested stepping up SUD’s efforts to cut back on unaccounted for water loss. Unaccounted for water loss is the difference between the amount of water treated at the plant and amount registered as sold on customer meters, meaning water SUD is not paid for. Recent testing revealed only one line leak as a possible source of water loss. The other possible cause of the unaccounted for loss is meter inaccuracy. Beavers will research the cost of meter testing to determine if testing to find the source of the unaccounted for loss will pay for itself in revenue increase.
In addition to revenue loss, SUD is experiencing another problem due to the pandemic: increased flushing of disposable towelettes and masks. The towelettes and masks clog wastewater pumps and screens, driving up costs. “That’s what’s been killing our grinder pumps,” Beavers said. “A new screen cost $100,000.”
“Nothing needs to go down the toilet that’s not toilet paper or waste,” Smith said. The board is considering paid advertisements to publicize the problem.
Taking up another pandemic issue, the board agreed to allow University researchers to test wastewater for presence of the virus. Beavers noted EPA tests showed the virus is not transported by water or wastewater. The purpose of the testing would be to determine viral load trends once the students return. SUD will require a release from liability and notification when the testing will take place.
Southern Tennessee Regional Health System EASES VISITOR RESTRICTIONS
Limited visitation now available for most patients as elective and non-urgent procedures gradually resume
Winchester, Tennessee (May 21, 2020) – Southern Tennessee Regional Health System announced today that it is transitioning from a zero-visitor protocol to limited visitor restrictions as the hospital gradually resumes elective and non-urgent cases and services at its facilities. The decision was made as current projections continue to indicate a lower than expected volume of COVID-19 in the region and after careful review of state and federal guidance. Effective, Tuesday, May 26, 2020 updated restrictions, which will now allow most patients to have one visitor or support person per day, will be implemented.
“Our hospital’s top priority is safeguarding the health and wellbeing of our patients, providers, employees and community,” said Cliff Wilson, chief executive officer (CEO) of Southern Tennessee Regional Health System. “We continue to monitor closely the prevalence of the virus in our community as we adapt our operations to safely care for and support our patients, and we feel confident that it is safe to begin allowing limited visitors again at this time.”
As part of the updated visitor restrictions, ICU and med-surg patients will be limited to one well visitor per day (cannot be rotated, must be the same individual for the respective day). One well companion for outpatient appointments and one well support person for obstetric patients will also be permitted (cannot be rotated, must be the same individual for the respective day).
All visitors must be 12 years of age or older, will be screened upon entry and are required to wear a mask and a sticker while in the facility. Visitors who do not pass the screening at entry will be asked to reschedule their visit until they are symptom-free. Visitors are not allowed for high-risk, isolation, immunocompromised or respiratory patients who are under observation or test positive for COVID-19. Additionally, visitors are not allowed for Same-Day Surgery patients and Skilled Care, Senior Advantage, and Inpatient Rehab units (some approved exceptions may apply - e.g. pediatric patients, POA, and those receiving end-of-life care).
Southern Tennessee Regional Health System continues to screen everyone who enters the facility for symptoms consistent with COVID-19, per CDC guidelines. For additional updates on how the hospital is working to maintain a safe and supportive environment during the COVID-19 pandemic, please visit SouthernTnWinchester.com.
About Southern Tennessee Regional Health System
Part of LifePoint Health, Southern Tennessee Regional Health System (STRHS) is a regional network of hospitals and health care services serving the healthcare needs of communities in the southern Tennessee region with facilities in Winchester, Sewanee, Pulaski, and Lawrenceburg. The system has 382 licensed beds, more than 300 affiliated physicians, 1,250 employees, and serves more than 160,000 people in rural communities in the region. The Winchester campus provides inpatient and outpatient services to Franklin County and the surrounding area at its 131-bed acute care facility and physician practices. For more information, visit http://southerntennessee.com.
From the CDC: Considerations for Restaurants and Bars
Updated May 18, 2020
As restaurants and bars resume operations in some areas of the United States, CDC offers the following considerations for ways in which operators can protect employees, customers, and communities and slow the spread of COVID-19. Restaurants and bars can determine, in collaboration with state and local health officials, whether and how to implement these considerations, making adjustments to meet the needs and circumstances of the local community. Implementation should be guided by what is feasible, practical, acceptable, and tailored to the needs of each community. These considerations are meant to supplement—not replace—any state, local, territorial, or tribal health and safety laws, rules, and regulations with which businesses must comply.
Guiding Principles to Keep in Mind
The more an individual interacts with others, and the longer that interaction, the higher the risk of COVID-19 spread. The risk of COVID-19 spread increases in a restaurant or bar setting as follows:
- Lowest Risk: Food service limited to drive-through, delivery, take-out, and curb-side pick up.
- More Risk: Drive-through, delivery, take-out, and curb-side pick up emphasized. On-site dining limited to outdoor seating. Seating capacity reduced to allow tables to be spaced at least 6 feet apart.
- Even More Risk: On-site dining with both indoor and outdoor seating. Seating capacity reduced to allow tables to be spaced at least 6 feet apart.
- Highest Risk: On-site dining with both indoor and outdoor seating. Seating capacity notreduced and tables not spaced at least 6 feet apart.
COVID-19 is mostly spread by respiratory droplets released when people talk, cough, or sneeze. It is thought that the virus may spread to hands from a contaminated surface and then to the nose or mouth, causing infection. Therefore, personal prevention practices (such as handwashing, staying home when sick) and environmental cleaning and disinfection are important principles that are covered in this document. Fortunately, there are a number of actions operators of restaurants and bars can take to help lower the risk of COVID-19 exposure and spread.
Promoting Behaviors that Reduce Spread
Restaurants and bars may consider implementing several strategies to encourage behaviors that reduce the spread of COVID-19 among employees and customers.
- Staying Home when Appropriate
- Educate employees about when they should stay home and when they can return to work.
- Actively encourage employees who are sick or have recently had a close contact with a person with COVID-19 to stay home. Develop policies that encourage sick employees to stay at home without fear of reprisal, and ensure employees are aware of these policies.
- Employees should stay home if they have tested positive for or are showing COVID-19 symptoms.
- Employees who have recently had a close contact with a person with COVID-19 should also stay home and monitor their health.
- CDC’s criteria can help inform when employees they may return to work:
- Educate employees about when they should stay home and when they can return to work.
- Hand Hygiene and Respiratory Etiquette
- Require frequent employee handwashing (e.g. before, during, and after preparing food; after touching garbage) with soap and water for at least 20 seconds and increase monitoring to ensure adherence.
- Encourage employees to cover coughs and sneezes with a tissue. Used tissues should be thrown in the trash and hands washed immediately with soap and water for at least 20 seconds.
- If soap and water are not readily available, use hand sanitizer that contains at least 60% alcohol.
- Cloth Face Coverings
- Require the use of cloth face coverings among all staff, as feasible. Face coverings are mostessential in times when physical distancing is difficult. Information should be provided to staff and students on proper use, removal, and washing of cloth face coverings.
- Note: Cloth face coverings should not be placed on:
- Babies and children younger than 2 years old
- Anyone who has trouble breathing or is unconscious
- Anyone who is incapacitated or otherwise unable to remove the cloth face covering without assistance
- Note: Cloth face coverings should not be placed on:
- Cloth face coverings are meant to protect other people in case the wearer is unknowingly infected but does not have symptoms. Cloth face coverings are not surgical masks, respirators, or personal protective equipment.
- Require the use of cloth face coverings among all staff, as feasible. Face coverings are mostessential in times when physical distancing is difficult. Information should be provided to staff and students on proper use, removal, and washing of cloth face coverings.
- Adequate Supplies
- Ensure adequate supplies to support healthy hygiene behaviors. Supplies include soap, hand sanitizer containing at least 60% alcohol (placed on every table, if supplies allow), paper towels, tissues, disinfectant wipes, cloth face coverings (as feasible), and no-touch/foot pedal trash cans.
- Signs and Messages
- Post signs in highly visible locations (e.g., at entrances, in restrooms) that promote everyday protective measurespdf iconpdf icon and describe how to stop the spreadpdf iconpdf icon of germs such as by properly washing hands and properly wearing a cloth face coveringimage iconimage icon.
- Include messages (for example, videos) about behaviors that prevent spread of COVID-19 when communicating with vendors, staff, and customers (such as on business websites, in emails, and on social media accounts).
- Find free CDC print and digital resources at the bars and restaurant page, as well as on CDC’s communications resources main page.
Maintaining Healthy Environments
Restaurants and bars may consider several implementing strategies to maintain healthy environments.
- Cleaning and Disinfection
- Clean and disinfect frequently touched surfaces (e.g., door handles, cash registers, workstations, sink handles, bathroom stalls) at least daily, or as much as possible and as required by food safety requirements. Clean shared objects (e.g., payment terminals, tables, countertops/bars, receipt trays, condiment holders) between each use.
- Continue to follow all required safety laws, regulations, and rules.
- Use products that meet EPA disinfection criteriaexternal icon and that are appropriate for the surface. Allow the disinfectant to remain on the surface for the contact time recommended by the manufacturer.
- Establish a disinfection routine and train staff on proper cleaning timing and procedures to ensure safe and correct application of disinfectants.
- Wash, rinse, disinfect, and then sanitize food contact surfaces, food preparation surfaces, and food preparation equipment.
- Ensure that cleaning or disinfecting product residues are not left on table surfaces. Residues could cause allergic reactions or cause someone to ingest the chemicals.
- Develop a schedule for increased, routine cleaning and disinfection.
- Ensure safe and correct use and storage of disinfectants to avoid food contamination and harm to employees and other individuals. This includes storing products securely away from children.
- Use gloves when removing garbage bags or handling and disposing of trash. Wash handsafter removing gloves.
- Clean and disinfect frequently touched surfaces (e.g., door handles, cash registers, workstations, sink handles, bathroom stalls) at least daily, or as much as possible and as required by food safety requirements. Clean shared objects (e.g., payment terminals, tables, countertops/bars, receipt trays, condiment holders) between each use.
- Shared Objects
- Discourage sharing of items that are difficult to clean, sanitize, or disinfect.
- Limit any sharing of food, tools, equipment, or supplies by staff members.
- Ensure adequate supplies to minimize sharing of high-touch materials (e.g., serving spoons) to the extent possible; otherwise, limit use of supplies and equipment by one group of workers at a time and clean and disinfect between use.
- Avoid using or sharing items that are reusable, such as menus, condiments, and any other food containers. Instead, use disposable or digital menus, single serving condiments, and no-touch trash cans and doors.
- Use touchless payment options as much as possible, if available. Ask customers and employees to exchange cash or card payments by placing on a receipt tray or on the counter rather than by hand to avoid direct hand to hand contact. Clean and disinfectfrequently touched surfaces such as pens, counters, or hard surfaces between use and encourage patrons to use their own pens.
- Use disposable food service items (e.g., utensils, dishes, napkins, tablecloths). If disposable items are not feasible or desirable, ensure that all non-disposable food service items are handled with gloves and washed with dish soap and hot water, or in a dishwasher. Employees should wash their hands after removing their gloves or after handling used food service items.
- Avoid use of food and beverage utensils and containers brought in by customers.
- Ventilation
- Ensure that ventilation systems operate properly and increase circulation of outdoor air as much as possible, for example by opening windows and doors and prioritizing outdoor seating. Do not open windows and doors if doing so poses a safety or health risk to customers or employees (e.g., risk of falling or triggering asthma symptoms).
- Water Systems
- To minimize the risk of Legionnaires’ disease and other diseases associated with water, take steps to ensure that all water systems and features (e.g., sink faucets, decorative fountains, drinking fountains) are safe to use after a prolonged facility shutdown.
- Modified Layouts and Procedures
- Change restaurant and bar layouts to ensure that all customer parties remain at least 6 feet apart (e.g., marking tables/stools that are not for use).
- Limit seating capacity to allow for social distancing.
- Offer drive-through, curbside take out, or delivery options as applicable. Prioritize outdoor seating as much as possible.
- Ask customers to wait in their cars or away from the establishment while waiting to pick up food or when waiting to be seated. Inform customers of food pickup and dining protocols on the business’ website and on posted signs.
- Discourage crowded waiting areas by using phone app, text technology, or signs to alert patrons when their table is ready. Avoid using “buzzers” or other shared objects.
- Consider options for dine-in customers to order ahead of time to limit the amount of time spent in the establishment.
- Avoid offering any self-serve food or drink options, such as buffets, salad bars, and drink stations.
- Physical Barriers and Guides
- Install physical barriers, such as sneeze guards and partitions, particularly in areas where it is difficult for individuals to remain at least 6 feet apart. Barriers can be useful in restaurant kitchens and at cash registers, host stands, or food pickup areas where maintaining physical distance of at least 6 feet is difficult.
- Provide physical guides, such as tape on floors or sidewalks and signage, to ensure that individuals remain at least 6 feet apart. Consider providing these guides where lines form, in the kitchen, and at the bar.
- Communal Spaces
- Close shared spaces such as break rooms, if possible; otherwise stagger use and clean and disinfect between use.
Maintaining Healthy Operations
Restaurants and bars may consider implementing several strategies to maintain healthy operations.
- Protections for Employees at Higher Risk for Severe Illness from COVID-19
- Offer options for employees at higher risk for severe illness (including older adults and people of all ages with certain underlying medical conditions) that limits their exposure risk (e.g., modified job responsibilities such as managing inventory rather than working as a cashier, or managing administrative needs through telework).
- Consistent with applicable law, develop policies to protect the privacy of persons at higher risk for severe illness in accordance with applicable privacy and confidentiality laws and regulations.
- Regulatory Awareness
- Be aware of local or state policies and recommendations related to group gatherings to determine if events can be held.
- Staggered or Rotated Shifts and Sittings
- Rotate or stagger shifts to limit the number of employees in the restaurant or bar at the same time.
- Stagger and limit dining times to minimize the number of customers in the establishment.
- When possible, use flexible worksites (e.g., telework) and flexible work hours (e.g., staggered shifts) to help establish policies and practices for social distancing (maintaining distance of approximately 6 feet) between employees and others, especially if social distancing is recommended by state and local health authorities.
- Gatherings
- Avoid group events, gatherings, or meetings where social distancing of at least 6 feet between people cannot be maintained.
- Travel and Transit
- Encourage employees who use mass transit to consider using other transportation options (e.g., walking or biking, driving or riding by car- alone or with household members only) if feasible
- Designated COVID-19 Point of Contact
- Designate a staff person for each shift to be responsible for responding to COVID-19 concerns. All staff members should know who this person is and how to contact them..
- Communication Systems
- Put systems in place for:
- Consistent with applicable law and privacy policies, having staff self-report to the establishment’s point of contact if they have symptoms of COVID-19, a positive test for COVID-19, or were exposed to someone with COVID-19 within the last 14 days in accordance with health information sharing regulations for COVID-19external icon(e.g. see “Notify Health Officials and Close Contacts” in the Preparing for When Someone Gets Sick section below), and other applicable privacy and confidentiality laws and regulations.
- Notifying staff, customers, and the public of business closures, and restrictions in place to limit COVID-19 exposure (e.g., limited hours of operation).
- Consistent with applicable law and privacy policies, having staff self-report to the establishment’s point of contact if they have symptoms of COVID-19, a positive test for COVID-19, or were exposed to someone with COVID-19 within the last 14 days in accordance with health information sharing regulations for COVID-19external icon(e.g. see “Notify Health Officials and Close Contacts” in the Preparing for When Someone Gets Sick section below), and other applicable privacy and confidentiality laws and regulations.
- Put systems in place for:
- Leave (Time Off) Policies
- Implement flexible sick leave policies and practices that enable employees to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Examine and revise policies for leave, telework, and employee compensation.
- Leave policies should be flexible and not punish people for taking time off and should allow sick employees to stay home and away from co-workers. Leave policies should also account for employees who need to stay home with their children if there are school or childcare closures, or to care for sick family members.
- Develop policies for return-to-work after COVID-19 illness. CDC’s criteria to discontinue home isolation can inform these policies.
- Implement flexible sick leave policies and practices that enable employees to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Back-Up Staffing Plan
- Monitor absenteeism of employees, cross-train staff, and create a roster of trained back-up staff.
- Staff Training
- Train all employees in safety actions.
- Conduct training virtually, or ensure that social distancing is maintained during training.
- Recognize Signs and Symptoms
- Conduct daily health checks (e.g., temperature screening and/or or symptom checking) of staff safely and respectfully, and in accordance with any applicable privacy laws and regulations.
- Consider using examples of screening methods in CDC’s General Business FAQs as a guide.
- Conduct daily health checks (e.g., temperature screening and/or or symptom checking) of staff safely and respectfully, and in accordance with any applicable privacy laws and regulations.
- Support Coping and Resilience
- Promote employees eating healthy, exercising, getting sleep, and finding time to unwind.
- Encourage employees to talk with people they trust about their concerns and how they are feeling.
- Consider posting signs for the national distress hotline: 1-800-985-5990, or text TalkWithUs to 66746
Preparing for Sick Employees
Restaurants and bars may consider implementing several strategies to prepare for when someone gets sick.
- Advise Sick Employees of Home Isolation Criteria
- Communicate to sick employees that they should not return to work until they have met CDC’s criteria to discontinue home isolation.
- Isolate and Transport Those Who are Sick
- Make sure that employees know they should not come to work if they are sick, and they should notify their manager or other designated COVID-19 point of contact if they become sick with COVID-19 symptoms, test positive for COVID-19, or have been exposed to someone with COVID-19 or have been exposed to someone with COVID-19 symptoms or a confirmed or suspected case.
- Immediately separate employees or customers with COVID-19 symptoms (i.e., fever, cough, shortness of breath). Individuals who are sick should go home or to a healthcare facility, depending on how sever their symptoms are, and follow CDC guidance for caring for oneself and others who are sick.
- Clean and Disinfect
- Close off areas used by a sick person and do not use these areas until after cleaning and disinfecting them.
- Wait at least 24 hours before cleaning and disinfecting. If 24 hours is not feasible, wait as long as possible. Ensure safe and correct use and storage of cleaning and disinfection productsexternal icon, including storing them securely away from children.
- Notify Health Officials and Close Contacts
- In accordance with state and local laws, restaurant and bar operators should notify local health officials and staff immediately of any case of COVID-19 among employees, while maintaining confidentiality in accordance with the Americans with Disabilities Act (ADA)external icon.
- Advise those who have had close contact with a person diagnosed with COVID-19 to stay home and self-monitor for symptoms, and follow CDC guidance if symptoms develop. Critical infrastructure workers may refer to CDC Guidance for Critical Infrastructure Workers, if applicable.
Other Resources
Cloth Face Coverings
- Require the use of cloth face coverings among all staff, as feasible. Face coverings are mostessential in times when physical distancing is difficult. Information should be provided to staff and students on proper use, removal, and washing of cloth face coverings.
- Note: Cloth face coverings should not be placed on:
- Babies and children younger than 2 years old
- Anyone who has trouble breathing or is unconscious
- Anyone who is incapacitated or otherwise unable to remove the cloth face covering without assistance
- Note: Cloth face coverings should not be placed on:
- Cloth face coverings are meant to protect other people in case the wearer is unknowingly infected but does not have symptoms. Cloth face coverings are not surgical masks, respirators, or personal protective equipment.
Adequate Supplies
- Ensure adequate supplies to support healthy hygiene behaviors. Supplies include soap, hand sanitizer containing at least 60% alcohol (placed on every table, if supplies allow), paper towels, tissues, disinfectant wipes, cloth face coverings (as feasible), and no-touch/foot pedal trash cans.
Signs and Messages
- Post signs in highly visible locations (e.g., at entrances, in restrooms) that promote everyday protective measurespdf icon and describe how to stop the spreadpdf icon of germs such as by properly washing hands and properly wearing a cloth face coveringimage icon.
- Include messages (for example, videos) about behaviors that prevent spread of COVID-19 when communicating with vendors, staff, and customers (such as on business websites, in emails, and on social media accounts).
- Find free CDC print and digital resources at the bars and restaurant page, as well as on CDC’s communications resources main page.
From the CDC: Considerations for Institutes of Higher Education
Updated May 21, 2020
As some institutes of higher education (IHE) open in the United States, the Centers for Disease Control and Prevention (CDC) offers the following considerations for ways in which IHEs can help protect students and employees (e.g., faculty, staff, and administrators) and slow the spread of the Coronavirus Disease 2019 (COVID-19). IHEs vary considerably in geographic location, size, and structure. As such, IHE officials can determine, in collaboration with state and local health officials, whether and how to implement these considerations while adjusting to meet the unique needs and circumstances of the IHE and local community. Implementation should be guided by what is feasible, practical, acceptable, and tailored to the needs of each community. Health facilities managed by the IHE may refer to CDC’s Guidance for U.S. Healthcare Facilities and may find it helpful to reference the Ten Ways Healthcare Systems Can Operate Effectively During the COVID-19 Pandemic. These considerations are meant to supplement—not replace—any state, local, territorial, or tribal health and safety laws, rules, and regulations with which IHEs must comply.
Guiding Principles to Keep in Mind
The more an individual interacts with others, and the longer that interaction, the higher the risk of COVID-19 spread. The risk of COVID-19 spread increases in IHE non-residential and residential (i.e., on-campus housing) settings as follows:
IHE General Settings
- Lowest Risk: Faculty and students engage in virtual-only learning options, activities, and events.
- More Risk: Small in-person classes, activities, and events. Individuals remain spaced at least 6 feet apart and do not share objects (e.g., hybrid virtual and in-person class structures or staggered/rotated scheduling to accommodate smaller class sizes).
- Highest Risk: Full-sized in-person classes, activities, and events. Students are not spaced apart, share classroom materials or supplies, and mix between classes and activities.
IHE On-Campus Housing Settings
- Lowest Risk: Residence halls are closed, where feasible.
- More Risk: Residence halls are open at lower capacity and shared spaces are closed (e.g., kitchens, common areas).
- Highest Risk: Residence halls are open at full capacity including shared spaces (e.g., kitchens, common areas).
COVID-19 is mostly spread by respiratory droplets released when people talk, cough, or sneeze. It is thought that the virus may spread to hands from a contaminated surface and then to the nose or mouth, causing infection. Therefore, personal prevention practices (such as handwashing, staying home when sick) and environmental prevention practices (such as cleaning and disinfection) are important principles that are covered in this document. Fortunately, there are a number of actions IHE administrators can take to help lower the risk of COVID-19 exposure and spread.
Promoting Behaviors that Reduce Spread
IHEs may consider implementing several strategies to encourage behaviors that reduce the spread of COVID-19.
- Staying Home or Self-Isolating when Appropriate
- If a decision is made to have any version of in-person classes, before returning to campus, actively encourage students, faculty, and staff who have been sick with COVID-19 symptoms, tested positive for COVID-19, or have been potentially exposed to someone with COVID-19 (either through community-related exposure or international travel) to follow CDC guidance to self-isolate or stay home.
- Once back on campus, educate students, faculty, and staff on when they should stay home or self-isolate in their living quarters.
- Actively encourage students, faculty, and staff who are sick or have recently had a close contact with a person with COVID-19 to stay home or in their living quarters (e.g., dorm room). Develop policies that encourage sick individuals to stay at home without fear of reprisals, and ensure students, faculty, and staff are aware of these policies. Offer virtual learning and telework options, if feasible.
- Students, faculty, and staff should stay home when they have tested positive for or are showing symptoms of COVID-19.
- Students, faculty, and staff who have recently had a close contact with a person with COVID-19 should also stay home and monitor their health.
- CDC’s criteria can help inform return to work/school policies:
- Hand Hygiene and Respiratory Etiquette
- Recommend and reinforce handwashing with soap and water for at least 20 seconds.
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used.
- Encourage students, faculty, and staff to cover coughs and sneezes with a tissue or use the inside of your elbow. Used tissues should be thrown in the trash and hands washed immediately with soap and water for at least 20 seconds.
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used.
- Recommend and reinforce handwashing with soap and water for at least 20 seconds.
- Cloth Face Coverings
- Recommend and reinforce use of cloth face coverings among students, faculty, and staff. Face coverings should be worn as feasible and are most essential in times when physical distancing is difficult. Individuals should be frequently reminded not to touch the face covering and to wash their hands frequently. Information should be provided to all students, faculty, and staff on proper use, removal, and washing of cloth face coverings.
- Note: Cloth face coverings should not be placed on:
- Babies and children younger than 2 years old
- Anyone who has trouble breathing or is unconscious
- Anyone who is incapacitated or otherwise unable to remove the cover without assistance
- Cloth face coverings are meant to protect other people in case the wearer is unknowingly infected but does not have symptoms. Cloth face coverings are not surgical masks, respirators, or other medical personal protective equipment.
- Note: Cloth face coverings should not be placed on:
- Recommend and reinforce use of cloth face coverings among students, faculty, and staff. Face coverings should be worn as feasible and are most essential in times when physical distancing is difficult. Individuals should be frequently reminded not to touch the face covering and to wash their hands frequently. Information should be provided to all students, faculty, and staff on proper use, removal, and washing of cloth face coverings.
- Adequate Supplies
- Support healthy hygiene behaviors by providing adequate supplies, including soap, hand sanitizer containing at least 60 percent alcohol, paper towels, tissues, disinfectant wipes, cloth face coverings (as feasible), and no-touch/foot pedal trash cans.
- Signs and Messages
- Post signs in highly visible locations (e.g., building entrances, restrooms, dining areas) that promote everyday protective measurespdf icon and describe how to stop the spreadpdf iconof germs (such as by properly washing hands and properly wearing a cloth face coveringimage icon).
- Include messages (for example, videos) about behaviors that prevent spread of COVID-19 when communicating with faculty, staff, and students (such as on IHE websites, in emails, and on IHE social media accounts) in accordance with the Clery Actexternal icon.
- Find freely available CDC print and digital resources on CDC’s communications resources main page.
Maintaining Healthy Environments
IHEs may consider implementing several strategies to maintain healthy environments.
- Cleaning and Disinfection
- Clean and disinfect frequently touched surfaces (e.g., door handles, sink handles, drinking fountains, grab bars, hand railings, bathroom stalls, dining hall tables) within IHE facilities at least daily or between use as much as possible. Use of shared objects (e.g., lab equipment, computer equipment, desks) should be limited when possible, or cleaned between use.
- If transport vehicles (e.g., buses) are used by the IHE, drivers should practice all safety actions and protocols as indicated for other staff (e.g., hand hygiene, cloth face coverings). To clean and disinfect IHE buses, vans, or other vehicles, see guidance for bus transit operators.
- Develop a schedule for increased, routine cleaning and disinfection.
- Ensure safe and correct use and storage of cleaners and disinfectantsexternal icon, including storing products securely. Use products that meet EPA disinfection criteriaexternal icon.
- Encourage students, faculty, and staff to keep their personal items (e.g., cell phones, other electronics) and personal work and living spaces clean. Encourage students, faculty, and staff to use disinfectant wipes to wipe down shared desks, lab equipment, and other shared objects and surfaces before use.
- Ensure there is adequate ventilation when using cleaning products to prevent students or staff from inhaling toxic fumes.
- Shared Objects
- Discourage sharing of items that are difficult to clean or disinfect.
- Ensure adequate supplies to minimize sharing of high-touch materials to the extent possible (e.g., assigning each student their own art supplies, lab equipment, computers) or limit use of supplies and equipment by one group of students at a time and clean and disinfect between use.
- Avoid sharing electronic devices, books, pens, and other learning aids.
- Ventilation
- Ensure ventilation systems operate properly and increase circulation of outdoor air as much as possible, for example by opening windows and doors. Do not open windows and doors if doing so poses a safety or health risk (e.g., risk of falling, triggering asthma symptoms) to students, faculty, or staff using the facility.
- Water Systems
- To minimize the risk of Legionnaires’ disease and other diseases associated with water, take steps to ensure that all water systems and features (e.g., sink faucets, drinking fountains, decorative fountains) are safe to use after a prolonged facility shutdown. Drinking fountains should be cleaned and disinfected, but encourage faculty, staff and students to bring their own water to minimize use and touching of water fountains.
- Modified Layouts
- Space seating/desks at least 6 feet apart when feasible. For lecture halls, consider taping off seats and rows to ensure six-foot distance between seats.
- Host smaller classes in larger rooms.
- Offer distance learning in addition to in-person classes to help reduce the number of in-person attendees.
- Provide adequate distance between individuals engaged in experiential learning opportunities (e.g., labs, vocational skill building activities).
- Create distance between students in IHE vehicles (e.g., skipping rows) when possible.
- Physical Barriers and Guides
- Install physical barriers, such as sneeze guards and partitions, particularly in areas where it is difficult for individuals to remain at least 6 feet apart (e.g., cash registers).
- Provide physical guides, such as tape on floors or sidewalks and signs on walls to ensure that individuals remain at least 6 feet apart in lines and at other times.
- Communal Spaces
- Close shared spaces such as dining halls, game rooms, exercise rooms, and lounges if possible; otherwise, stagger use and restrict the number of people allowed in at one time to ensure everyone can stay at least 6 feet apart, and clean and disinfect between use.
- Add physical barriers, such as plastic flexible screens, between bathroom sinks and between beds especially when they cannot be at least 6 feet apart.
- For more information on communal spaces in student or faculty housing (e.g., laundry rooms, shared bathrooms and recreation areas) follow CDC’s guidance for Shared or Congregate Housing.
- Food Service
- Provide grab-and-go options for meals. If a cafeteria or group dining room is typically used, if possible, serve individually plated meals (versus buffet or any self-serve stations).
- Use disposable food service items (e.g., utensils, dishes). If disposable items are not feasible or desirable, ensure that all non-disposable food service items are handled with gloves and washed with dish soap and hot water or in a dishwasher. Individuals should wash their hands after removing their gloves or after directly handling used food service items.
- If food is offered at any event, have pre-packaged boxes or bags for each attendee instead of a buffet or family-style meal. Avoid sharing food and utensils and consider the safety of individuals with food allergies.pdf icon
Maintaining Healthy Operations
IHEs may consider implementing several strategies to maintain healthy operations.
- Protections for Students, Faculty, and Staff at Higher Risk for Severe Illness from COVID-19
- Offer options for faculty and staff at higher risk for severe illness (including older adults and people of all ages with certain underlying medical conditions) that limit their exposure risk (e.g., telework and modified job responsibilities).
- Offer options for students at higher risk for severe illness that limit their exposure risk (e.g. virtual learning opportunities).
- Consistent with applicable law, put in place policies to protect the privacy of people at higher risk for severe illness regarding underlying medical conditions in compliance with applicable federal and state privacy and confidentiality laws.
- Regulatory Awareness
- Be aware of state or local regulatory agency policies related to group gatherings to determine if events can be held.
- Gatherings
- Pursue virtual group events, gatherings, or meetings, if possible, and promote social distancing of at least 6 feet between people if events are held. Limit group size to the extent possible.
- Pursue options to convene sporting events and participate in sports activities in ways that reduce the risk of transmission of COVID-19 to players, families, coaches, and communities.
- Limit any nonessential visitors, volunteers, and activities involving external groups or organizations as possible – especially with individuals who are not from the local geographic area (e.g., community, town, city, or county).
- Telework and Virtual Meetings
- Encourage telework for as many faculty and staff as possible, especially employees at higher risk for severe illness from COVID-19.
- Replace in-person meetings with video- or tele-conference calls whenever possible.
- Provide student support services virtually, as feasible.
- When possible, use flexible work or learning sites (e.g., telework, virtual learning) and flexible work or learning hours (e.g., staggered shifts or classes) to help establish policies and practices for social distancing (maintaining distance of approximately 6 feet) between people, especially if social distancing is recommended by state and local health authorities.
- Travel and Transit
- Consider options for limiting non-essential travel in accordance with state and local regulations and guidance.
- Encourage students, faculty and staff who use mass transit to consider using other transportation options (e.g., walking, biking, driving or riding by car- alone or with household members only) if feasible.
- Designated COVID-19 Point of Contact
- Designate an administrator or office to be responsible for responding to COVID-19 concerns. All IHE students, faculty and staff should know who this person is and how to contact them.
- Participation in Community Response Efforts
- Consider participating with state or local authorities in broader COVID-19 community response efforts (e.g., sitting on community response committees).
- Communication Systems
- Put systems in place for:
- Consistent with applicable law and privacy policies, having students, faculty and staff report to the IHE if they have symptoms of COVID-19, a positive test for COVID-19, or were exposed to someone with COVID-19 within the last 14 days in accordance with health information sharing regulations for COVID-19 external icon(e.g. see “Notify Health Officials and Close Contacts” in the Preparing for When Someone Gets Sick section below), and other applicable federal and state privacy and confidentiality laws, such as the Family Educational Rights and Privacy Act (FERPA).
- Notifying faculty, staff, students, families, and the public of IHE closures and any restrictions in place to limit COVID-19 exposure (e.g., limited hours of operation).
- Put systems in place for:
- Leave (Time Off) and Excused Absence Policies
- Implement flexible sick leave policies and practices that enable faculty, staff, and students to stay home or self-isolate when they are sick, have been exposed, or caring for someone who is sick.
- Examine and revise policies for excused absences and virtual learning (students) and leave, telework, and employee compensation (employees).
- Leave and excused absence policies should be flexible, not be punitive to people for taking time off and should allow sick employees and students to stay home and away from others. Leave and excused absence policies should also account for employees and students who need to stay home with their children if there are school or childcare closures, or to care for sick family members.
- Develop policies for returning to classes and IHE facilities after COVID-19 illness. CDC’s criteria to discontinue home isolation and quarantine can inform these policies.
- Implement flexible sick leave policies and practices that enable faculty, staff, and students to stay home or self-isolate when they are sick, have been exposed, or caring for someone who is sick.
- Back-Up Staffing Plan
- Monitor absenteeism of employees and students, cross-train staff, and create a roster of trained back-up staff.
- Staff Training
- Train staff on all safety protocols
- Conduct training virtually or ensure that social distancing is maintained during training.
- Recognize Signs and Symptoms
- If feasible, conduct daily health checks or ask faculty, staff, and students to conduct self-checks (e.g., temperature screening and/or symptom checking).
- Health checks should be done safely and respectfully, and in accordance with any applicable federal or state privacy and confidentiality laws and regulations. IHE administrators may use examples of screening methods found in CDC’s General Business FAQs.
- Sharing Facilities
- Encourage any organizations that share or use IHE facilities to also follow these considerations.
- Support Coping and Resilience
- Encourage employees and students to take breaks from watching, reading, or listening to news stories, including social media if they are feeling overwhelmed or distressed.
- Promote employees and students eating healthy, exercising, getting sleep and finding time to unwind.
- Encourage employees and students to talk with people they trust about their concerns and how they are feeling.
- Consider posting signages for the national distress hotline: 1-800-985-5990, or text TalkWithUs to 66746
Preparing for When Someone Gets Sick
IHEs may consider implementing several strategies to prepare for when someone gets sick.
- Advise Sick Individuals of Home Isolation Criteria
- Sick faculty, staff, or students should not return to in-person classes or IHE facilities, or end isolation until they have met CDC’s criteria to discontinue home isolation.
- Isolate and Transport Those Who are Sick
- Make sure that faculty, staff, and students know they should not come to the IHE if they are sick, and should notify IHE officials (e.g., IHE designated COVID-19 point of contact) if they become sick with COVID-19 symptoms, test positive for COVID-19, or have been exposed to someone with COVID-19 symptoms or a confirmed or suspected case.
- Immediately separate faculty, staff, and students with COVID-19 symptoms (such as fever, cough, or shortness of breath). Individuals who are sick should go home or to a healthcare facility, depending on how severe their symptoms are, and follow CDC Guidance for caring for oneself and others who are sick. IHEs may follow CDC’s Guidance for Shared or Congregate Housing for those that live in IHE housing.
- Work with IHE administrators and healthcare providers to identify an isolation room, area, or building/floor (for on-campus housing) to separate anyone who has COVID-19 symptoms or tests positive but does not have symptoms. IHE healthcare providers should use Standard and Transmission-Based Precautions when caring for sick people. See: What Healthcare Personnel Should Know About Caring for Patients with Confirmed or Possible COVID-19 Infection.
- Establish procedures for safely transporting anyone who is sick to their home or to a healthcare facility. If you are calling an ambulance or bringing someone to the hospital, try to call first to alert them that the person may have COVID-19.
- Clean and Disinfect
- Close off areas used by a sick person and do not use these areas until after cleaning and disinfecting
- Wait at least 24 hours before cleaning and disinfecting. If 24 hours is not feasible, wait as long as possible. Ensure safe and correct use and storage of cleaning and disinfection productsexternal icon, including storing products securely away from children.
- Notify Health Officials and Close Contacts
- In accordance with applicable federal, state and local laws and regulations, IHEs should notify local health officials, faculty, staff, and students immediately of any case of COVID-19 while maintaining confidentiality in accordance with the Americans with Disabilities Act (ADA)external icon, FERPA or and other applicable laws and regulations.
- Inform those who have had close contact with a person diagnosed with COVID-19 to stay home or in their living quarters and self-monitor for symptoms, and follow CDC guidanceif symptoms develop.
From the CDC:Considerations for Youth Sports
As some communities in the United States begin to start youth sports activities again, the Centers for Disease Control and Prevention (CDC) offers the following considerations for ways in which youth sports organizations can protect players, families, and communities and slow the spread of the Coronavirus Disease 2019 (COVID-19). Administrators of youth sports organizations can consult with state and local health officials to determine if and how to put into place these considerations. Each community may need to make adjustments to meet its unique needs and circumstances. Implementation should be guided by what is practical, acceptable, and tailored to the needs of each community. These considerations are meant to supplement – not replace – any state, local, territorial, or tribal health and safety laws, rules, and regulations with which youth sports organizations must comply.
Guiding Principles to Keep in Mind
There are a number of actions youth sports organizations can take to help lower the risk of COVID-19 exposure and reduce the spread during competition and practice. The more people a child or coach interacts with, the closer the physical interaction, the more sharing of equipment there is by multiple players, and the longer that interaction, the higher the risk of COVID-19 spread. Therefore, risk of COVID-19 spread can be different, depending on the type of activity. The risk of COVID-19 spread increases in youth sports settings as follows:
- Lowest Risk: Performing skill-building drills or conditioning at home, alone or with family members.
- Increasing Risk: Team-based practice.
- More Risk: Within-team competition.
- Even More Risk: Full competition between teams from the same local geographic area.
- Highest Risk: Full competition between teams from different geographic areas.
If organizations are not able to keep in place safety measures during competition (for example, maintaining social distancing by keeping children six feet apart at all times), they may consider dropping down a level and limiting participation to within-team competition only (for example, scrimmages between members of the same team) or team-based practices only. Similarly, if organizations are unable to put in place safety measures during team-based activities, they may choose individual or at-home activities, especially if any members of the team are at high-risk for severe illness.
Assessing Risk
The way sports are played, and the way equipment is shared can influence the spread of COVID-19 among players. When you are assessing the risk of spread in your sport, consider:
- Physical closeness of players, and the length of time that players are close to each other or to staff. Sports that require frequent closeness between players may make it more difficult to maintain social distancing, compared to sports where players are not close to each other. For close-contact sports (e.g., wrestling, basketball), play may be modified to safely increase distance between players.
- For example, players and coaches can:
- focus on individual skill building versus competition;
- limit the time players spend close to others by playing full contact only in game-time situations;
- decrease the number of competitions during a season.
- For example, players and coaches can:
- Amount of necessary touching of shared equipment and gear (e.g., protective gear, balls, bats, racquets, mats, or water bottles). It is also possible that a person can get COVID-19 by touching a surface or object that has the virus on it, and then touching their own mouth, nose, or eyes. Minimize equipment sharing, and clean and disinfect shared equipment between use by different people to reduce the risk of COVID-19 spread.
- Ability to engage in social distancing while not actively engaged in play (e.g., during practice, on the sideline, or in the dugout). During times when players are not actively participating in practice or competition, attention should be given to maintaining social distancing by increasing space between players on the sideline, dugout, or bench. Additionally, coaches can encourage athletes to use downtime for individual skill-building work or cardiovascular conditioning, rather than staying clustered together.
- Age of the player. Older youth might be better able to follow directions for social distancing and take other protective actions like not sharing water bottles. If feasible, a coach, parent, or other caregiver can assist with making sure that athletes maintain proper social distancing. For younger athletes, youth sports programs may ask parents or other household members to monitor their children and make sure that they follow social distancing and take other protective actions (e.g., younger children could sit with parents or caregivers, instead of in a dugout or group area).
- Players at higher risk of developing serious disease. Parents and coaches should assess level of risk based on individual players on the team who may be at higher risk for severe illness, such as children who may have asthma, diabetes, or other health problems.
- Size of the team. Sports with a large number of players on a team may increase the likelihood of spread, compared to sports with fewer team members. Consider decreasing team sizes, as feasible.
- Nonessential visitors, spectators, volunteers. Limit any nonessential visitors, spectators, volunteers, and activities involving external groups or organizations.
- Travel outside of the local community. Traveling outside of the local community may increase the chances of exposing players, coaches, and fans to COVID-19, or unknowingly spreading it to others. This is the case particularly if a team from an area with high levels of COVID-19 competes with a team from an area with low levels of the virus. Youth sports teams should consider competing only against teams in their local area (e.g., neighborhood, town, or community).
Promoting Behaviors that Reduce Spread
Youth sports organizations may consider implementing several strategies to encourage behaviors that reduce the spread of COVID-19.
- Staying Home when Appropriate
- Educate staff and player families about when they should stay home and when they can return to activity
- Actively encourage sick staff, families, and players to stay home. Develop policies that encourage sick employees to stay at home without fear of reprisal, and ensure employees aware of these policies.
- Individuals, including coaches, players, and families, should stay home if they have tested positive for or are showing COVID-19 symptoms.
- Individuals, including coaches, players, and families, who have recently had a close contact with a person with COVID-19 should also stay home and monitor their health.
- CDC’s criteria can help inform return to work/school policies:
- Educate staff and player families about when they should stay home and when they can return to activity
- Hand Hygiene and Respiratory Etiquette
- Teach and reinforce handwashing with soap and water for at least 20 seconds
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used (for staff and older children who can safely use hand sanitizer).
- Do not allow spitting and encourage everyone to cover their coughs and sneezes with a tissue or use the inside of their elbow. Used tissues should be thrown in the trash and hands washed immediately with soap and water for at least 20 seconds.
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used.
- Teach and reinforce handwashing with soap and water for at least 20 seconds
- Cloth Face Coverings
- Teach and reinforce the use of cloth face coverings. Face coverings are not intended to protect the wearer, but rather to reduce the risk of spreading COVID-19 from the person wearing the mask (who may not have any symptoms of disease). Face coverings may be challenging for players (especially younger players) to wear while playing sports. Face coverings should be worn by coaches, youth sports staff, officials, parents, and spectators as much as possible.
- Wearing cloth face coverings is most important when physical distancing is difficult.
- People wearing face coverings should be reminded to not touch the face covering and to wash their hands frequently. Information should be provided to all participants on the proper use, removal, and washing of cloth face coverings.
- Note: Cloth face coverings should not be placed on:
- Babies and children younger than 2 years old;
- Anyone who has trouble breathing or is unconscious;
- Anyone who is incapacitated or otherwise unable to remove the cloth face covering without assistance.
- Note: Cloth face coverings should not be placed on:
- Adequate Supplies
- If hand washing facilities are available, support healthy hygiene by providing supplies including soap, paper towels, tissues, and no-touch/foot pedal trash cans. If hand washing facilities are not available, provide hand sanitizer with at least 60% alcohol (for coaches, staff and older players who can safely use hand sanitizer).
- Signs and Messages
- Post signs in highly visible locations (e.g., at entrances and exits, and in restrooms) that promote everyday protective measurespdf icon and describe how to stop the spreadpdf icon of germs such as by properly washing hands and properly wearing a cloth face coveringimage icon.
- Broadcast regular announcements on public announcement (PA) system
- Include COVID-19 prevention messages (for example, videos) about behaviors that prevent spread of COVID-19 when communicating with staff, volunteers, officials, and families. This could include links, videos, and prevention messages in emails, on organization websites, and through the team and league’s social media accounts.
- Find freely available CDC print and digital resources on CDC’s communication resourcesmain page.
Maintaining Healthy Environments
Youth sports organizations may consider implementing several strategies to maintain healthy environments.
- Cleaning and Disinfection
- Clean and disinfect frequently touched surfaces on the field, court, or play surface (e.g., drinking fountains) at least daily, or between uses as much as possible. Use of shared objects and equipment (e.g., balls, bats, gymnastics equipment) should be limited, or cleaned between use by each individual if possible.
- Develop a schedule for increased, routine cleaning and disinfection.
- Ensure safe and correct use and storage of disinfectants, including storing products securely away from children. Use products that meet EPA disinfection criteriaexternal icon.
- Identify an adult staff member or volunteer to ensure proper cleaning and disinfection of objects and equipment, particularly for any shared equipment or frequently touched surfaces.
- Cleaning products should not be used near children, and staff should ensure that there is adequate ventilation when using these products to prevent children or themselves from inhaling toxic fumes.
- Use gloves when removing garbage bags or handling and disposing of trash. Wash hands after removing gloves.
- Shared Objects
- Discourage sharing of items that are difficult to clean, sanitize, or disinfect. Do not let players share towels, clothing, or other items they use to wipe their faces or hands.
- Make sure there are adequate supplies of shared items to minimize sharing of equipment to the extent possible (e.g., protective gear, balls, bats, water bottles); otherwise, limit use of supplies and equipment to one group of players at a time and clean and disinfect between use.
- Keep each player’s belongings separated from others’ and in individually labeled containers, bags, or areas.
- If food is offered at any event, have pre-packaged boxes or bags for each attendee instead of a buffet or family-style meal. Avoid sharing food and utensils. Offer hand sanitizer or encourage hand washing.
- Ventilation
- If playing inside, ensure ventilation systems or fans operate properly. Increase circulation of outdoor air as much as possible, for example by opening windows and doors. Do not open windows and doors doing so poses a safety or health risk (e.g., risk of falling or triggering asthma symptoms) to players or others using the facility.
- Water Systems
- To minimize the risk of Legionnaires’ disease and other diseases associated with water, take steps to ensure that all water systems and features (e.g., drinking fountains, decorative fountains) are safe to use after a prolonged facility shutdown. Drinking fountains should be cleaned and disinfected but encourage staff and players to bring their own water to minimize touching water fountains.
- Modified Layouts and Social (Physical) Distancing
- Identify adult staff members or volunteers to help maintain social distancing among youth, coaches, umpires/referees, and spectators (if state and local directives allow for spectators).
- Space players at least 6 feet apart on the field while participating in the sport (e.g., during warmup, skill building activities, simulation drills)
- Discourage unnecessary physical contact, such as high fives, handshakes, fist bumps, or hugs.
- Prioritize outdoor, as opposed to indoor, practice and play as much as possible.
- Create distance between players when explaining drills or the rules of the game.
- If keeping physical distance is difficult with players in competition or group practice, consider relying on individual skill work and drills.
- Encourage players to wait in their cars with guardians until just before the beginning of a practice, warm-up, or game, instead of forming a group.
- Limit the use of carpools or van pools. When riding in an automobile to a sports event, encourage players to ride to the sports event with persons living in their same household.
- If practices or competition facilities must be shared, consider increasing the amount of time between practices and competitions to allow for one group to leave before another group enters the facility. If possible, allow time for cleaning and/or disinfecting.
- Physical Barriers and Guides
- Provide physical guides, such as signs and tape on floors or playing fields, to make sure that coaches and players remain at least 6 feet apart.
- Communal Spaces
- Close shared spaces such as locker rooms, if possible; otherwise, stagger use and clean and disinfect between use.
- Limit the number of players sitting in confined player seating areas (e.g., dugouts) by allowing players to spread out into spectator areas if more space is available (e.g., if spectators are not allowed).
Maintaining Healthy Operations
Youth sports organizations may consider implementing several strategies to maintain healthy operations.
- Protections for Staff and Players at Higher Risk for Severe Illness from COVID-19
- Offer options for individuals at higher risk of severe illness from COVID-19 (risk increases with age, and people of any age with certain medical conditions are at higher risk), such as virtual coaching and in-home drills that limits their exposure risk.
- Limit youth sports participation to staff and youth who live in the local geographic area (e.g., community, city, town, or county) to reduce risk of spread from areas with higher levels of COVID-19.
- Regulatory Awareness
- Be aware of state or local regulatory agency policies related to group gatherings to determine if events can be held.
- Identifying Small Groups and Keeping them Together (Cohorting)
- Keep players together in small groups with dedicated coaches or staff, and make sure that each group of players and coach avoid mixing with other groups as much as possible. Teams might consider having the same group of players stay with the same coach or having the same group of players rotate among coaches.
- Consider staging within-team scrimmages instead of playing games with other teams to minimize exposure among players and teams.
- Staggered Scheduling
- Stagger arrival and drop-off times or locations by cohort (group) or put in place other protocols to limit contact between groups and with guardians as much as possible. One example is increasing the amount of time between practices and competitions to allow for one group to depart before another group enters the facility. This also allows for more time to clean the facility between uses.
- When possible, use flexible worksites (e.g., telework) and flexible work hours (e.g., staggered shifts) to help establish policies and practices for social distancing (maintaining a distance of approximately 6 feet) between employees and others, especially if social distancing is recommended by state and local health authorities.
- Gatherings, Spectators, and Travel
- Avoid group events, such as games, competitions, or social gatherings, where spacing of at least 6 feet between people cannot be maintained.
- Limit any nonessential visitors, spectators, volunteers, and activities involving external groups or organizations as much as possible – especially with individuals not from the local geographic area (e.g., community, town, city, or county).
- Avoid activities and events such as off-site competitions or excursions (e.g., watching a professional team compete).
- Designated COVID-19 Point of Contact
- Designate a youth sports program staff person to be responsible for responding to COVID-19 concerns. All coaches, staff, officials, and families should know who this person is and how to contact them.
- Communication Systems
- Put systems in place for:
- Consistent with applicable law and privacy policies, having coaches, staff, umpires/officials, and families of players (as feasible) self-report to the youth sports organization if they have symptoms of COVID-19, a positive test for COVID-19, or were exposed to someone with COVID-19 within the last 14 days in accordance with health information sharing regulations for COVID-19external icon (e.g. see “Notify Health Officials and Close Contacts” in the Preparing for When Someone Gets Sick section below), and other applicable laws and regulations.
- Notifying staff, officials, families, and the public of youth sports facility closures and restrictions in place to limit COVID-19 exposure (e.g., limited hours of operation).
- Put systems in place for:
- Leave (Time Off) Policies
- Implement flexible sick leave policies and practices for coaches, officials, and staff that enable employees to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Examine and revise policies for leave, telework, and employee compensation.
- Leave policies should be flexible and not be punitive to people for taking time off and should allow sick employees to stay home and away from co-workers. Leave policies should also account for employees who need to stay home with their children if there are school or childcare closures, or to care for sick family members.
- Develop policies for return-to-play after COVID-19 illness. CDC’s criteria to discontinue home isolation and quarantine can inform these policies.
- Implement flexible sick leave policies and practices for coaches, officials, and staff that enable employees to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Back-up Staffing Plan
- Monitor absenteeism of coaches and officials, cross-train staff, and create a roster of trained back-up personnel.
- Coach and Staff Training
- Train coaches, officials, and staff on all safety protocols.
- Conduct training virtually, or ensure that social distancing is maintained during training.
- Recognize Signs and Symptoms
- If feasible, conduct daily health checks (e.g., symptom checking) of coaches, officials, staff, and players safely and respectfully, and in accordance with any applicable privacy and confidentiality laws and regulations.
- Youth sports program administrators may use examples of screening methods found in CDC’s supplemental Guidance for Child Care Programs that Remain Open as a guide for screening children, and CDC’s General Business FAQs for screening staff.
- Sharing Facilities
- Encourage any organizations that share or use the youth sports facilities to also follow these considerations.
- Support Coping and Resilience
- Encourage employees to take breaks from watching, reading, or listening to news stories, including social media if they are feeling overwhelmed or distressed.
- Promote healthy eating, exercising, getting sleep, and finding time to unwind.
- Encourage employees to talk with people they trust about their concerns and how they are feeling.
- Consider posting signs for the national distress hotline: 1-800-985-5990, or text TalkWithUs to 66746
Preparing for When Someone Gets Sick
Youth sports organizations may consider implementing several strategies to prepare for when someone gets sick.
- Advise Sick Individuals of Home Isolation Criteria
- Sick coaches, staff members, umpires/officials, or players should not return until they have met CDC’s criteria to discontinue home isolation.
- Isolate and Transport Those Who are Sick
- Make sure that coaches, staff, officials, players, and families know that sick individuals should not attend the youth sports activity, and that they should notify youth sports officials (e.g., the COVID-19 point of contact) if they (staff) or their child (families) become sick with COVID-19 symptoms, test positive for COVID-19, or have been exposed to someone with COVID-19 symptoms or a confirmed or suspected case.
- Immediately separate coaches, staff, officials, and players with COVID-19 symptoms (i.e., fever, cough, shortness of breath) at any youth sports activity. Individuals who are sick should go home or to a healthcare facility, depending on how severe their symptoms are, and follow CDC guidance for caring for oneself and others who are sick. Individuals who have had close contact with a person who has symptoms should be separated and sent home as well, and follow CDC guidance for community-related exposure (see “Notify Health Officials and Close Contacts” below). If symptoms develop, individuals and families should follow CDC guidance for caring for oneself and others who are sick.
- Establish procedures for safely transporting anyone who is sick to their home or to a healthcare facility. If you are calling an ambulance or bringing someone to the hospital, try to call first to alert them that the person may have COVID-19.
- Clean and Disinfect
- Close off areas used by a sick person and do not use these areas until after cleaning and disinfecting them (for outdoor areas, this includes surfaces or shared objects in the area, if applicable).
- Wait at least 24 hours before cleaning and disinfecting. If 24 hours is not feasible, wait as long as possible. Ensure safe and correct use and storage of cleaningexternal icon and disinfection products, including storing them securely away from children.
- Notify Health Officials and Close Contacts
- In accordance with state and local privacy and confidentiality laws and regulations, youth sports organizations should notify local health officials, youth sports program staff, umpires/officials, and families immediately of any case of COVID-19 while maintaining confidentiality in accordance with the Americans with Disabilities Act (ADA)external icon and other applicable laws and regulations.
- Work with local health officials to develop a reporting system (e.g., letter) youth sports organizations can use to notify health officials and close contacts of cases of COVID-19.
- Advise those who have had close contact with a person diagnosed with COVID-19 to stay home and self-monitor for symptoms, and to follow CDC guidance if symptoms develop.

















